Central Sleep Apnea or CSA
August 29th, 2009
Central Sleep Apnea (CSA) information on this page includes:-
- General Information on Central Sleep Apnea
- Central Sleep Apnea Diagnosis
- Central Sleep Apnea Treatment
About Central Sleep Apnea
Central Sleep Apnea is a less common form of Sleep Apnea.
Central Sleep Apnea symptoms are usually characterized by brief interruptions of breathing during sleep and you have significant pauses in breathing or shallow breaths while you sleep.
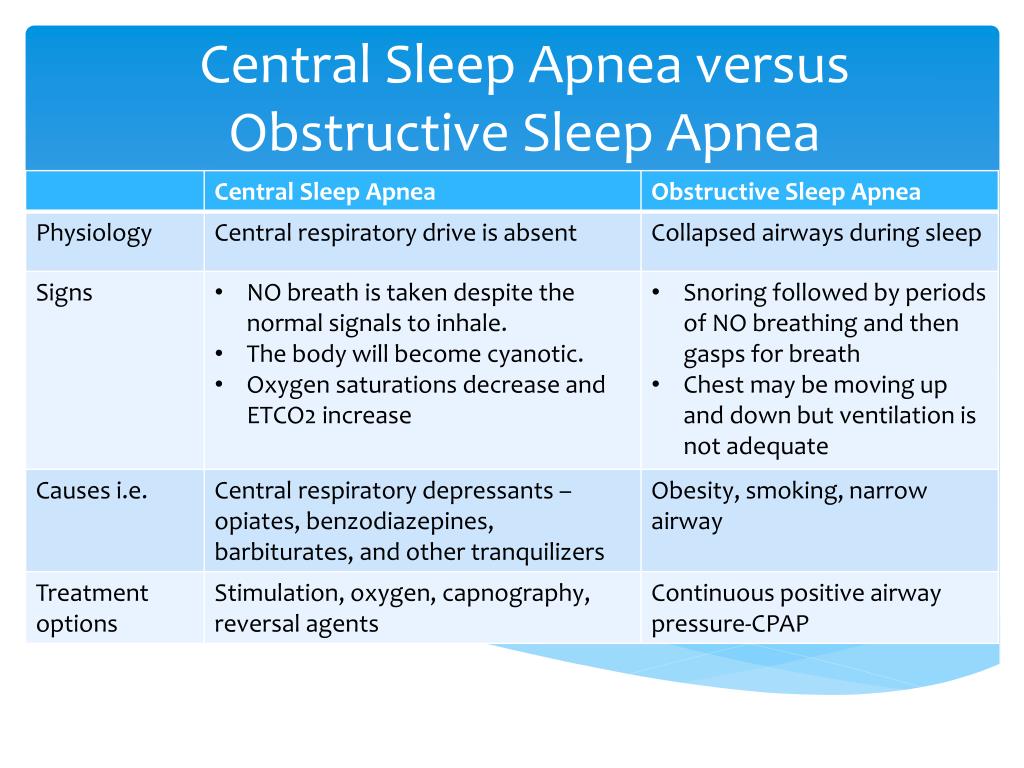
Central Sleep Apnea causes can be varied but it usually occurs when the area of your brain that controls your breathing doesn’t send the correct signals to your breathing muscles and you make no effort to breathe for brief periods. This usually continues until the oxygen level in your blood stream depletes to a critical level triggering a strong enough stimuli to the brain to restart your breathing.
Under normal circumstances when the brain senses a lack of oxygen or an excess of carbon dioxide in the blood, it will speed up breathing to increase the intake of oxygen and as a result reduces the levels of carbon dioxide in the blood stream.
In reality these breathing pauses can last from a few seconds to minutes usually with a change in the heart rate, reduction in blood oxygen, and in some cases for infants a general relaxation of the body’s muscles (called hypotonia). The Apneas can often occur 5 to 30 times or more an hour with normal breathing then starting again, typically with a loud snort or choking sound and a body jerk.
For adults Central Sleep Apnea diagnosis can be associated with heart disease, use of some medications and being at increased/higher altitudes. In infants, it usually occurs with children that have been born prematurely or who have other congenital disorders.
For some people with heart disease they have increased concentrations of carbon dioxide in their blood at all times. In chronic and long term cases this sustained increase in blood carbon dioxide concentrations results in the brain ignoring blood oxygen levels and instead monitoring the blood carbon dioxide to determine when to take the next breath.
The bodies breathing responses to changes in carbon dioxide levels becomes slower leading to wide fluctuations in both carbon dioxide and oxygen concentrations in the blood as well as associated changes in the rates of breathing.
As carbon dioxide levels increase the brains responds by increasing the rate of breathing, but the brain being slow to adjust, continues to signal for more rapid breathing until the carbon dioxide level swings back in the other direction and becomes too low. Breathing then slows down or stops until the carbon dioxide level rises to a concentration that is high enough to again trigger the need to breathe. This pattern of abnormal breathing is called Cheyne-Stokes breathing (after the men who described it) and is characterised by repetitive cycles of fast breathing followed by slow breathing and apnea.
This Cheyne-Stokes breathing pattern can happen when awake or asleep, but becomes more of a problem when asleep.
You often move out of deep sleep and into a light sleep for brief moments of wakefulness when your breathing pauses during or restarts after a Central Sleep Apnea event. This results in poor sleep quality that makes you tired during the day.
Diagnosis of CSA
Central Sleep Apnea usually occurs in adults with other medical problems. In both adults and infant patient groups Central Sleep Apnea is usually initially suspected by the treating doctor.
Central Sleep Apnea is normally diagnosed following a sleep study that is usually completed at a sleep center under a controlled and monitored environment. During the sleep study recordings of brain activity, eye movement and other muscle activity, breathing and heart rate, as well as the amount of oxygen in the blood are measured throughout the night and the duration of the study.
Central Sleep Apnea Treatment
For adults with Central Sleep Apnea, the CSA is treated by managing the underlying heart disease, medication interaction, high altitude, or other primary cause.
In infants, Central Sleep Apnea is usually treated with an apnea alarm. This alarm monitors the infant’s breathing with sensors and sounds a loud alarm when the infant experiences an apnea. The alarm is designed to usually wake the infant and the parents. Most infants tend to “out-grow” the Central Sleep Apnea episodes with the alarm monitoring being stopped after the episodes cease. Monitoring may be needed for a longer periods for infants with other congenital problems that are causing the Central Sleep Apnea.
It should be noted that for infants, Central Sleep Apnea is not the same thing as Sudden Infant Death Syndrome (SIDS) in that Central Sleep Apnea is a diagnosed, ongoing and known condition that can be monitored and managed.
Find some more detailed reference material on Central Sleep Apnea HERE
